

The burden of HAI is estimated to be even higher in developing countries, with prevalence rates varying between 14.8 and 19.1%. This is associated with prolonged hospital stay and additional treatment, increased healthcare costs, long-term disability and excess mortality. An estimated 5–15 of every 100 hospitalized patients in developed countries acquire HAI while in hospital. Healthcare associated infection (HAI) is a major problem for patient safety. CQI with regular monitoring and feedback of HH performance can be an effective approach in improving HH compliance in public hospitals in Kenya. Training and mentorship on the importance of HH for all moments is needed to improve overall HH compliance. Adjusted HH compliance from all quarters improved from baseline, but comparing each quarter to the previous quarter, the improvement fluctuated over time. Wearing of gloves often replaced proper HH in surgical departments, which although not significant, had lower compliance compared to departments for internal medicine (aOR 0.93, 95% CI 0.85–1.02).
#5 moments of hand hygiene cdc professional
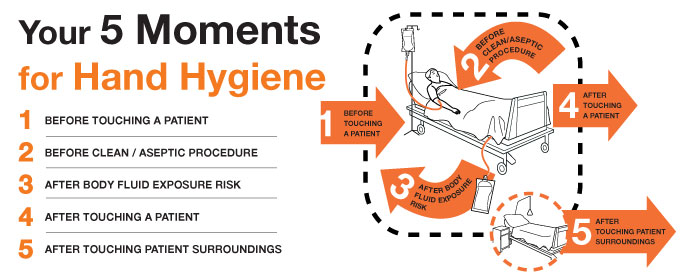
Adjusting for site, professional category and department, compliance was higher after a moment of body fluid exposure (aOR 1.43, 95% CI 1.17–1.74, p value < 0.001) and lower before an aseptic procedure (aOR 0.12, 95% CI 0.08–0.17, p value < 0.001) compared to after patient contact. Indication/moment for HH was significantly associated with compliance. Hand hygiene compliance improved from 27% at baseline to 44% after 21 months. Covariates were explored using mixed-effects logistic regression with random department-level intercepts. Healthcare workers trained on Infection Prevention and Control (IPC) observed and recorded HH opportunities and subsequent compliance among staff, including nurses, clinicians, and auxiliary staff, using the World Health Organization’s “ My Five Moments for Hand Hygiene” tool. Data were collected monthly between April 2018 and December 2019 in Thika and Kitale Hospitals. MethodsĪ CQI project targeting the improvement of hand hygiene was implemented, including training and mentorship. To determine the impact of the HH CQI program and identify factors associated with HH compliance between 20.

We implemented a continuous quality improvement (CQI) program targeting HH in two hospitals in Kenya. In low resource settings, models to improve HH compliance are needed. Hand hygiene (HH) is central in prevention of health care-associated infections.


 0 kommentar(er)
0 kommentar(er)
